- Multiple Copays For One Visit California
- 2 Copays For One Office Visit
- Two Copays For One Office Visit
- Multiple Copays For One Visit Form
- Multiple Copays For One Visit Without
- Multiple Copays One Visit
Copays Can Add Up Fast. Copayments add up. If you see the doctor frequently or fill prescriptions routinely, copayments that are credited toward your deductible will help (but again, remember that even if they're not counted towards your deductible, they're probably still counting towards your plan's maximum out-of-pocket amount). The video visit came with an 'administrative fee' of $50 that she would have had to pay upfront, she says — five times what the copay would have been for an in-person session. Re: Billing question - 2 copays for 1 office visit? I agree, that doesn't seem right. Had you seen your regular doctor and had a sonogram, you wouldn't have been charged twice. My eye doctor hit me with two copays, one for his visit and one for a specific test he ran. That didn't seem right, especially as it wasn't explained to me before hand. Physical therapy with insurance costs a co-pay of $20 to $55 per session or coinsurance of 10%-50% or more. Health insurance companies cover 50 to 75 percent of the costs when medically necessary. However, coverage begins after you've paid the yearly deductible, which ranges from $250 to $1,250 or more. Multiple myeloma is a type of cancer formed by cancerous plasma cells. Normal plasma cells are found in the bone marrow and are an important part of the body’s immune system. PAF Co-Pay Relief Program makes no representation as to the accuracy or any other aspect of the information contained on any website accessed from the CPR website.
Original Medicare is a federal health insurance program for seniors and people with certain disabilities. When a Medicare recipient requires emergency care, Medicare does cover emergency room visits for the most part, and the recipient pays a copayment.
Read on to learn more about emergency room costs and how a Medicare Supplement Insurance plan can help reduce what you pay out of pocket for Medicare emergency room coverage.
What is the Copay for Medicare Emergency Room Coverage?
A copay is the fixed amount that you pay for covered health services after your deductible is met. In most cases, a copay is required for doctor’s visits, hospital outpatient visits, doctor’s and hospital outpatients services, and prescription drugs. Medicare copays differ from coinsurance in that they're usually a specific amount, rather than a percentage of the total cost of your care.
Medicare does cover emergency room visits. You'll pay a Medicare emergency room copay for the visit itself and a copay for each hospital service. It is important to remember, however, that your actual Medicare urgent care copay amount can vary widely, depending on the services you require and where you receive care.

If you are admitted for inpatient hospital services after an emergency room visit, Medicare Part A does help cover costs for your hospital stay. Medicare Part A does not cover emergency room visits that don't result in admission for an inpatient hospital stay.
What Does Medicare Pay for Emergency Room Visits?
Multiple Copays For One Visit California
Medicare Part A emergency room coverage is specifically for inpatient hospital stays. If your emergency room visit requires you to be admitted for inpatient care, your Medicare Part A benefits would kick in but are subject to the Part A deductible and coinsurance.
Most ER services are considered hospital outpatient services, which are covered by Medicare Part B.They include, but are not limited to:
- Emergency and observation services, including overnight stays in a hospital
- Diagnostic and laboratory tests
- X-rays and other radiology services
- Some medically necessary surgical procedures
- Medical supplies and equipment, like splints, crutches and casts
- Preventive and screening services
- Certain drugs that you wouldn't administer yourself
NOTE: There's an important distinction to be made between inpatient and outpatient hospital statuses. Your hospital status affects how much you pay for services. Unless your doctor has written an order to admit you as an inpatient, you're an outpatient, even if you spend the night in the hospital.

How Medicare Part B Pays For Outpatient Services
2 Copays For One Office Visit
Medicare Part B pays for outpatient services like the ones listed above, under the Outpatient Prospective Payment System (OPPS). The OPPSpays hospitals a set amount of money (or payment rate) for the services they provide to Medicare beneficiaries.
The payment rate varies from hospital to hospital based on the costs associated with providing services in that area, and are adjusted for geographic wage variations.
Other Medicare Costs
Aside from Medicare ER copays, there are other outpatient hospital costs that you should be aware of when visiting the emergency room, such as deductibles and coinsurance. In most cases, if you receive care in a hospital emergency department and are covered by Medicare Part B, you'll also be responsible for:
- An annual Part B deductible of $203 (in 2021).
- A coinsurance payment of 20% of the Medicare-approved amount for most doctor’s services and medical equipment.
Two Copays For One Office Visit
How You Pay For Outpatient Services
In order for your Medicare Part B coverage to kick in, you must pay the yearly Part B deductible. Once your deductible is met, Medicare pays its share and you pay yours in the form of a copay or coinsurance.
Multiple Copays For One Visit Form
Get Help Covering Your Emergency Room Copay
If you're worried about a trip to the emergency room adding expensive and unpredictable costs to your health care budget, consider joining a Medicare Supplement Insurance (or Medigap) Plan. Medigap is private health insurance that Medicare beneficiaries can buy to cover costs that Medicare doesn't, including some copays. All Medigap plans cover at least a percentage of your Medicare Part B coinsurance or ER copay costs.
To find a Medigap plan in your area, call 1-800-995-4219 to connect with a licensed insurance agent.
Does Medicare Part A cover emergency room visits?
If you opted out of Medicare Part B, and only have Part A, you may be wondering if you can get coverage for an emergency room visit. Medicare Part A is designed for hospital insurance, meaning that it's benefits are generally used once admitted to the hospital.
Resource Center
Enter your email address and get a free guide to Medicare and Medicare Supplement Insurance.
By clicking 'Sign up now' you are agreeing to receive emails from MedicareSupplement.com.
We've been helping people find their perfect Medicare plan for over 10 years.
Ready to find your plan?
Multiple Copays For One Visit Without
multiple E/M
Multiple Copays One Visit
First, determine 'Who' is billing, the physician or the Facility (different rules)'
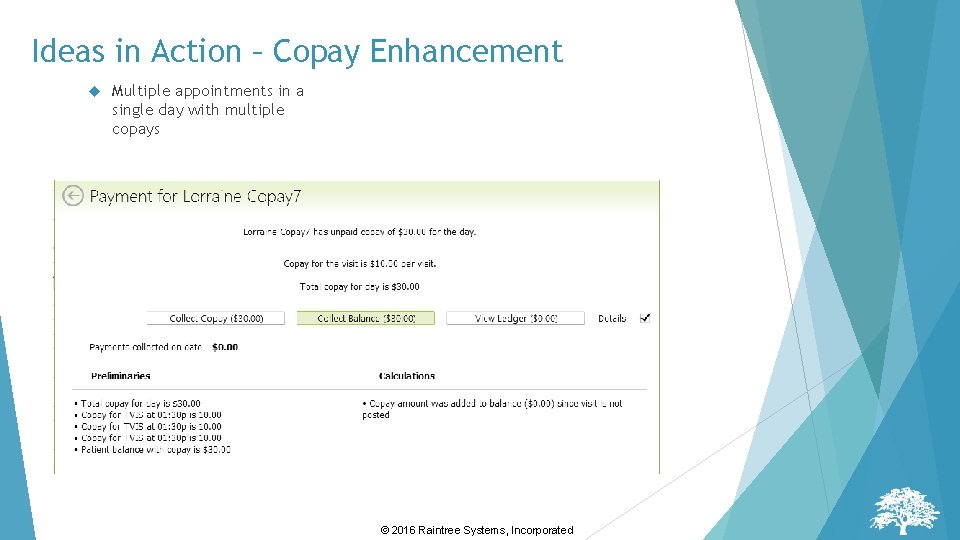
It is possible to bill for more than one E/M services, by multiple physicians within a single group practice, on the same date-of-service
• Medicare Claims Processing Manual, 100-04, Chapter 12, 30.6.5, Physicians in a group practice; “If more than one evaluation and management (face-to-face) service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported unless the evaluation and management services are for unrelated problems.”
• However, this should be an exception and not the norm (two separate E/M service classes).
Diagnosis Codes (Medical Necessity)
• ICD-9 official guidelines were developed to assist both the healthcare provider and the coder in identifying those diagnoses and procedures that are to be reported.
• The importance of consistent, complete documentation in the medical record cannot be overemphasized. Without such documentation accurate coding cannot be achieved.
• The entire record should be reviewed to determine the specific reason for the encounter and the conditions treated.
Facility Billing, not Physician Billing:
Billing Two Separate E/M Services
• Modifier 25 - Significant, Separately Identifiable Evaluation and Management Service by the same physician on the same day of Procedure or Other Service
• Modifier 27 – Multiple Outpatient Hospital E/M Encounters on the Same Date
– For hospital outpatient reporting purposes, utilization of hospital resources related to separate and distinct E/M encounters performed in multiple outpatient hospital settings on the same date may be reported by adding modifier 27 to each appropriate level outpatient and/or emergency department E/M code(s).
– This modifier provides a means of reporting circumstances involving evaluation and management services provided by physician(s) in more than one (multiple) outpatient hospital setting(s) (eg,hospital emergency department, clinic). Note: This modifier is not to be used for physician reporting of multiple E/M services performed by the same physician on the same date.
Facility Billing Two Separate E/M Services –Modifier 27 (not billed by physician)
Clinical Example
• Medicare patient is seen in a hospital outpatient clinic in the morning for a respiratory symptom and goes to the emergency room for an unrelated condition later in the day.
Another example is when a patient presents to the emergency room twice on the same day for unrelated visits.
• If the services are billed on a single claim, the appropriate Emergency Department E/M code and the appropriate level outpatient E/M code should be reported with modifier -27 appended. The G0 condition code should also be used to indicate that the hospital is aware that it is billing more than one clinic visit on the same day and that those encounters are unrelated; and therefore, qualify for separate reimbursement for each visit.
• For multiple claims, the hospital would bill the clinic services with the appropriate level outpatient E/M code with the modifier -27 appended, and the appropriate revenue and diagnosis code(s). Also, the hospital would bill the emergency room claim with the appropriate level emergency department E/M code, revenue code, diagnosis code(s), and other ancillary service(s) or procedure(s), as appropriate
CPT Assistant, December 2001
Communication with payor if you meet rules and are still being denied.
Nancy
